Understanding Status Epilepticus: A Medical Emergency
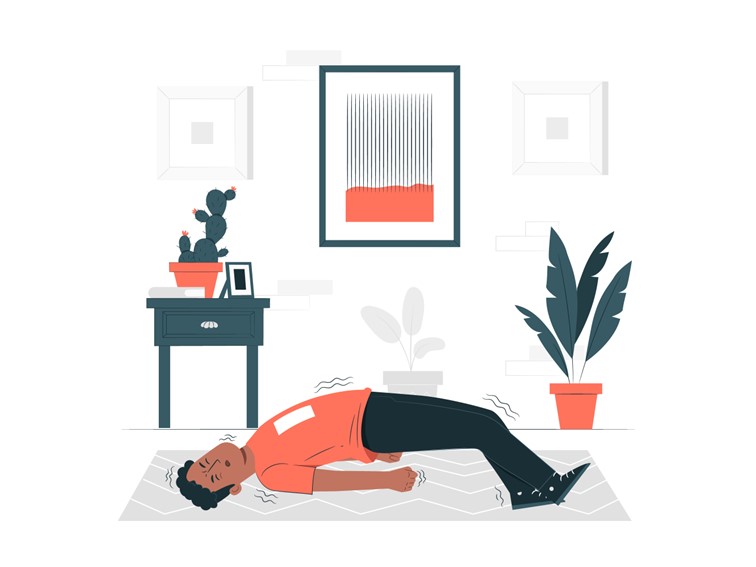
Status
epilepticus in children is a neurological emergency that demands immediate
medical attention. Characterized by prolonged or repeated seizures without full
recovery between episodes. Status epilepticus poses significant risks to the
brain and body. Let us try to understand the causes, symptoms, treatment
options, and long-term implications of this critical condition.
What is Status Epilepticus in Children?
1. In
simple terms, status epilepticus is a condition where seizures last longer than
five minutes or occur in rapid succession without the patient regaining
consciousness. It is broadly classified into two types:
2. Convulsive
Status Epilepticus (CSE): This involves prolonged
or recurrent tonic-clonic seizures, which are typically characterized by
jerking movements and muscle rigidity.
3. Non-Convulsive
Status Epilepticus (NCSE): This presents with
subtle or no motor symptoms and is often harder to diagnose. Patients may
appear confused, unresponsive, or display abnormal behavior.
Causes of Status Epilepticus
While SE can affect anyone, certain
factors increase its likelihood. Common causes include:
- Epilepsy:
Poorly managed or uncontrolled epilepsy is a major risk factor.
- Brain
Injuries: Trauma, stroke, or brain tumors
can trigger seizures.
- Infections:
Conditions such as meningitis, encephalitis, or systemic infections can
lead to status epilepticus in children.
- Metabolic
Imbalances: Hypoglycemia, hyponatremia, or
other electrolyte disturbances.
- Withdrawal:
Abrupt cessation of alcohol, benzodiazepines, or other medications.
- Drug
Use: Certain substances, including
recreational drugs, may provoke seizures.
- Unknown
Causes: In many cases, the exact cause
remains unidentified.
Symptoms to Watch For
The symptoms of status epilepticus in children depend on the type:
- Convulsive
SE: prolonged jerking movements, loss of
consciousness, difficulty breathing, and cyanosis (bluish skin
discoloration).
- Non-convulsive
SE: confusion, unresponsiveness,
disorientation, and subtle motor signs like lip-smacking or eye movements.
Why is SE dangerous?
Prolonged seizures can lead to severe complications, including:
- Brain
Damage: Continuous seizure activity can
damage brain cells.
- Respiratory
Issues: Difficulty breathing during
seizures can result in hypoxia (lack of oxygen).
- Cardiac
Stress: Elevated heart rate and blood
pressure can strain the cardiovascular system.
- Metabolic
disturbances: prolonged seizures
disrupt the body’s metabolic balance, leading to acidosis and other
issues.
- Mortality:
SE can be fatal if left untreated, with mortality rates ranging from 10%
to 20%, depending on the underlying cause and treatment.
Diagnosis
Diagnosing status epilepticus in children requires a combination of clinical observation and diagnostic tools:
- Electroencephalogram
(EEG): An essential tool to identify
seizure activity, especially in non-convulsive SE.
- Imaging:
CT scans or MRIs can help detect structural abnormalities in the brain.
- Blood
Tests: used to identify infections,
metabolic imbalances, or toxic substances.
Treatment Options
The primary goal of SE treatment is to stop seizures quickly while addressing the underlying cause. The treatment typically involves:
1.
Initial Stabilization
o Ensure
airway patency and provide oxygen.
o Monitor
vital signs and establish intravenous access.
2.
First-Line Medications
o Benzodiazepines
(e.g., lorazepam, diazepam) are the initial drugs of choice.
3.
Second-Line Medications
o If
seizures persist, antiepileptic drugs (AEDs) such as phenytoin, valproate, or
levetiracetam are administered.
4.
Refractory Status
Epilepticus
o In
cases where seizures continue despite treatment, patients may require
anesthetic agents like propofol or midazolam and admission to an intensive care
unit (ICU).
Prevention and Long-Term Management
For individuals with epilepsy or other risk factors, preventing SE involves:
- Adherence
to Treatment: Consistently taking
prescribed antiepileptic medications.
- Regular
Monitoring: Routine follow-ups with a
neurologist to adjust medication as needed.
- Avoiding
Triggers: Identifying and minimizing
seizure triggers, such as sleep deprivation or stress.
- Medical
Alert Devices: Wearing medical ID
bracelets or carrying cards to inform others of the condition.
Prognosis and Recovery
The outcome of status epilepticus in children largely depends on its cause, duration, and the timeliness of treatment. Early intervention improves the chances of full recovery, while delayed treatment increases the risk of long-term neurological damage.
Conclusion
Status epilepticus in children is a
life-threatening condition requiring prompt recognition and treatment. Public
awareness, proper management of epilepsy, and timely medical intervention are
crucial to improving outcomes for affected children. If you or someone you know
is at risk, understanding the signs and having a clear action plan can make all
the difference in an emergency.
For the comprehensive treatment of all
types of epilepsy in children, visit Dr. Habib’s Foster CDC – A renowned Child
Neuro Care Centre in Hyderabad.